Reference



Moonshot's Answer
Common variable immunodeficiency (CVID) is primarily characterized by B-cell defects, but it is also associated with several T-cell abnormalities. The main T-cell abnormalities in CVID include:
-
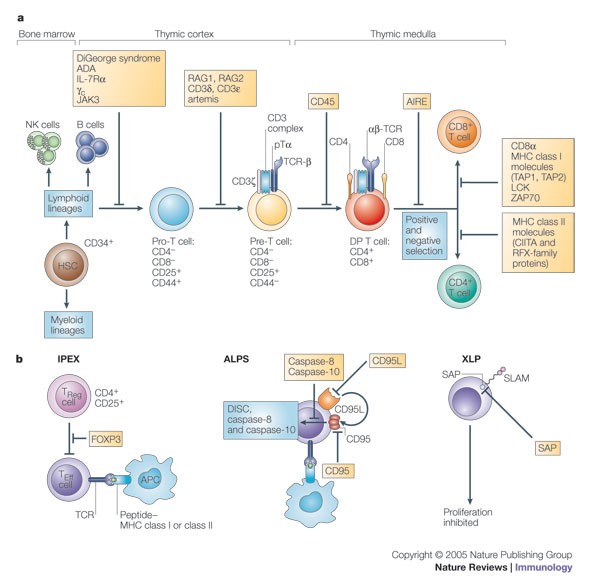
Decreased T-cell numbers: There is often a reduction in the total number of T cells, particularly in the CD4+ T helper subset, which is crucial for immune response regulation and B-cell function.
-
Impaired T-cell function: T cells in CVID patients may show impaired function, including reduced proliferation and cytokine production in response to stimuli.
-
Defective T-cell signaling: There can be defects in T-cell signaling pathways, which affect the activation and differentiation of T cells.
-
Altered T-cell subsets: There may be imbalances in the proportions of different T-cell subsets, such as increased proportions of naïve T cells and decreased proportions of memory T cells.
-
Autoimmunity: Some patients with CVID have T-cell abnormalities that contribute to autoimmune diseases, which can be associated with defects in regulatory T cells (Tregs).
-
Chronic T-cell activation: There is evidence of chronic T-cell activation in CVID, which may contribute to inflammation and tissue damage.
-
Defects in invariant NKT (iNKT) cells: Some studies have reported defects in iNKT cells, which are a unique subset of T cells that play a role in immune responses to certain pathogens and in immune regulation.
These abnormalities can contribute to the increased susceptibility to infections and the development of autoimmune diseases observed in CVID patients. Understanding these T-cell abnormalities is crucial for the management and treatment of CVID. For more detailed information, refer to the sources such as PubMed, JIACI, and Nature.
Follow Up
Related
What are the immunological abnormalities observed in ataxia-telangiectasia patients?
How can abnormal PrPSc protein be detected in brain tissue?
What type of papers are given priority by the Journal of Abnormal Psychology?
What are the major areas of focus for the Journal of Abnormal Psychology?