Reference



OpenAI's Answer
Prion diseases are challenging to diagnose based solely on symptoms due to several factors, as evidenced by current diagnostic practices and obstacles:
-
Non-Specific Symptoms: Prion diseases like Creutzfeldt-Jakob disease (CJD) present with a range of neurological symptoms such as rapidly progressive dementia, ataxia (loss of control of body movements), and myoclonus (involuntary muscle jerks) source. These symptoms are not unique to prion diseases and can be seen in other neurodegenerative conditions such as Alzheimer's and Parkinson's disease.
-
Overlap with Other Conditions: The clinical symptoms overlap significantly with many other neurodegenerative diseases, making differential diagnosis based on symptoms alone unreliable.
-
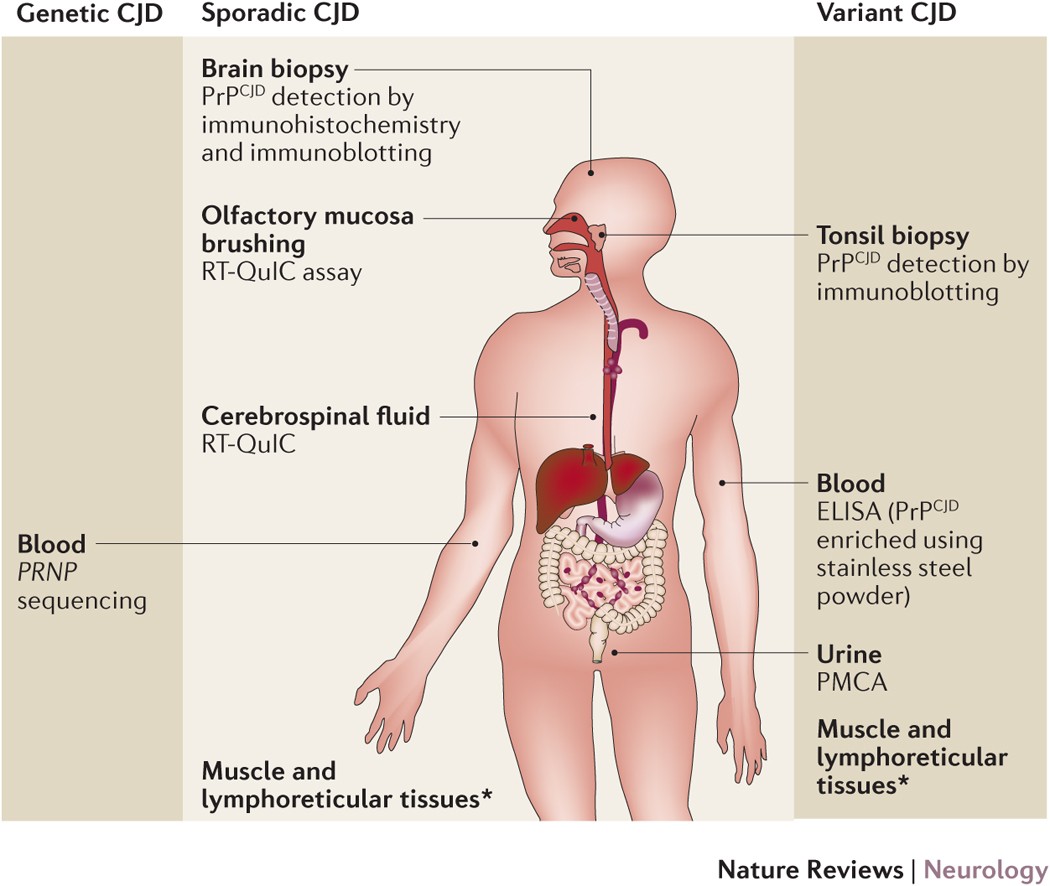
Lack of Definitive Biomarkers in Non-Invasive Tests: Although some auxiliary tests like cerebrospinal fluid (CSF) analysis, electroencephalogram (EEG), and MRI can support a clinical diagnosis, they are not definitive. The definitive diagnosis of prion diseases relies on detecting abnormal prion proteins in brain tissue, typically accomplished through a brain biopsy or post-mortem examination source.
-
Evolving Diagnostic Techniques: Advances in diagnostic approaches, like the real-time quaking-induced conversion (RT-QuIC) test, have improved the sensitivity and specificity of prion disease detection. However, these tests still need to be combined with clinical assessment and other diagnostic tools to reach a conclusive diagnosis source.
Diagnostic Methods
-
Clinical Evaluation: Initial diagnosis may include a thorough neurological examination and assessment of clinical history.
-
Auxiliary Tests:
- CSF Analysis: The presence of 14-3-3 protein, prion protein assays.
- EEG: Characteristic periodic sharp wave complex patterns.
- MRI: Diffusion-weighted imaging (DWI) showing specific patterns in the brain.
-
Definitive Diagnosis:
- Brain Biopsy: Examining brain tissue samples for the presence of abnormal prions.
- Post-Mortem Examination: Histological analysis confirming prion presence in brain tissue.
The complexity and the necessity for invasive procedures underline why prion diseases cannot be diagnosed based solely on symptoms.
For more detailed information, you can also visit resources like the John Hopkins Medicine website and this article on diagnostic measures.